Difficult Gallbladder – Part 2 The Technical Aspect
28th October 2023
https://youtu.be/wVLgoqqkNng?si=JiGev_8W_m01EjAN
The terminology used in this segment will be medically focused (aka more surgical terms). This segment will share some of my personal experience and techniques which I have used in the past. Some of the so called “exit strategy in a difficult case”.
a) Calot’s triangle – Calot first described the boundaries as the common hepatic duct, cystic duct and inferior surface of the liver. Current teaching in medical school is the common hepatic duct, cystic duct and cystic artery. During a difficult cholecystectomy the most challenging part is to dissect out Calot’s triangle. If we are able to do this part safely, the rest of the surgery becomes relatively easier.
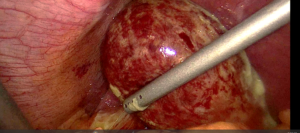
Surgical training teaches us to dissect this area as far away from the common bile duct as possible. This is quite easily done especially in the non infected gallbladder. Dissecting away from the common bile duct will reduce the risk of bile duct injuries (a serious complication of gallbladder surgery). However, when dealing with a necrotic or gangrenous gallbladder, the tissue around this area is often very friable or with gross inflammation caused by the infection. Dissecting through infected and inflamed tissue often causes lots of bleeding and the view is obscured.
One method which I use to overcome this is to dissect slightly closer to the common bile duct. The theory behind this technique is that the inflammation is caused by the infected gallbladder. When we are closer to the common bile duct and further away from the gallbladder, the tissue should have slightly less inflammation. Sometimes, I would encounter a “friendly” oedematous tissue that allow me to display the anatomy nicely.
b) What to do when we cannot display Calot’s triangle
Fundus first cholecystectomy is a technique which can be attempted in such cases. Fundus first cholecystectomy is not a new technique at all. In the open era of cholecystectomy, I have seen surgeons apply this technique routinely for all their cases. Current surgical teaching is not to use this technique as the first line approach because it does increase the risk of common bile duct injury.
The difficulty with this technique is how to identify the transition from gallbladder to cystic duct (especially in a infected gallbladder). One observation which I think is helpful is looking at the gallbladder fossa.
When dissecting the gallbladder off the liver, the gallbladder fossa will narrow down. When this narrowing is seen, I will dissect very close to the gallbladder. This will be the start of the gallbladder cystic duct junction.
c) Dissecting the gallbladder off the liver
In the western world, the teaching is generally to remove the whole gallbladder off the liver. I was taught to perform a subtotal (leaving the back wall of the gallbladder behind) cholecystectomy only during difficult cases. So the question is, what is a difficult case?
I studied and train in Australia. During my training days, I rarely encounter cirrhotic livers. This is more common in Asia because of the higher incidence of hepatitis B. During gallbladder surgery especially the infected ones, bleeding can be a problem. This is especially true in patients with liver cirrhosis. When dissecting an infected gallbladder off the liver, occasionally we may dissect into the liver parenchyma. This may result in bleeding which may be difficult to control. During my time in Singapore and various parts of Asia, I noticed that surgeons have a lower threshold of leaving the back wall of the gallbladder behind. Leaving the back wall behind reduces the risk of bleeding from the liver especially in cirrhotic livers.
d) Managing the cystic duct.
An important part of a gallbladder operation is closing the cystic duct. If the cystic duct is not closed properly, then bile will leak from the cystic stump. This complication can be a major problem especially if it is not identified early and managed well.
In cases where the cystic duct is of normal size, I would use hemalok clips to secure it. In the event when the cystic duct is thick and swollen, I will consider using a tie or an endoloop to close the cystic duct. When I am not able to get around the cystic duct or Hartmann’s pouch in badly infected cases, I would close cystic duct by suturing.
Last but not least, the surgeon has to ensure that here is no residual stones left in the remaining cystic duct. There are various techniques to manage this which is beyond the scope of this blog.
The techniques mentioned above are routinely used in my laparoscopic cholecystectomy cases. These techniques can easily be applied to the traditional open cholecystectomy as well.
Share this blog via:
- ← Difficult Gallbladder – Part 1 Identify the difficult cases
- Why do I need to fix my inguinal hernia? →